
Infection with the Zika virus during pregnancy can lead to neurological disorders, fetal abnormalities, and fetal death. Until now, it was unclear how the virus could cross the placenta, which nourishes the developing fetus and forms a strong barrier against microbes and chemicals that could harm the fetus. Researchers at Baylor College of Medicine, together with colleagues at Pennsylvania State University, report in Nature Communications on a strategy that allows the Zika virus to spread secretly in placental cells without alerting the immune system.
How Zika Virus Spreads Through the Human Placenta
“The mosquito-borne Zika virus triggered an epidemic in the Americas in 2015 that had reached 30 million cases by 2018,” said co-author Dr. Indira Mysorekar, E.I. Wagner Endowed, M.D., chair of internal medicine II, director of basic and translational research, and professor of medicine—infectious diseases at Baylor College of Medicine. “To prevent or control this devastating disease, it is crucial to understand how the Zika virus spreads through the human placenta and reaches the fetus.
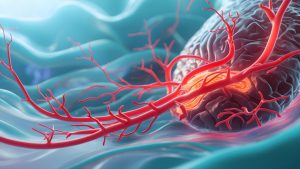
The researchers discovered that the Zika virus builds underground tunnels, a series of tiny tubes called tunnel nanotubes, which facilitate the transfer of virus particles to neighboring, uninfected cells. “We found that the formation of these tiny tunnels is controlled exclusively by a Zika protein called NS1,” said first author Dr. Rafael T. Michita, a postdoctoral fellow in the Mysorekar lab. “Exposure of placental cells to the NS1 protein of the Zika virus triggers tunnel formation. As the tunnels develop and connect neighboring cells, a pathway opens for the virus to infect new cells.“
Zika is the only virus in its family, which includes dengue and West Nile virus, among others, whose NS1 protein triggers tunnel formation in multiple cell types,” Michita said. Other viruses unrelated to Zika, such as HIV, herpes, influenza A, and SARS-CoV-2, the virus that causes COVID-19, can also induce tiny tunnels in the cells they infect and use these tunnels to spread to uninfected cells. This is the first time that tunnel formation has been detected in placental cells following Zika virus infection.
Important Findings that Contribute to the Development of Therapeutic Strategies
Interestingly, the tiny channels not only transported virus particles, but also RNA, proteins, and mitochondria, the main source of energy in a cell, from infected to neighboring cells. The researchers suspect that the transport of mitochondria through the tunnels gives the virus-infected cells an energy boost that promotes virus replication. They also show that movement through the tiny tunnels may help the Zika virus avoid triggering large-scale antiviral responses, such as the placenta’s interferon lambda (IFN-lambda) defense. Mutant Zika viruses that do not form tiny tunnels trigger a strong antiviral IFN-lambda response that may limit the spread of the virus.
“Overall, we show that the Zika virus uses a tunneling strategy to spread infection covertly in the placenta while hijacking mitochondria to promote its spread and survival. We suspect that this strategy also protects the virus from the immune response,“ said Mysorekar. ”These findings provide important insights that could be used to develop therapeutic strategies against this covert mode of transmission.”


